During the recent Dakar Rally, one of the riders who crashed sustained severe enough traumatic brain injury that he was placed in a medically induced coma. What does that really mean?
First, let’s look at what coma means. Coma describes an impaired level of consciousness when evaluated using a standard scoring system like the Glasgow Coma Scale for brain injury; coma is a score of eight or lower out of a maximum of 15 and a minimum of three. A GCS of three means that you are unresponsive — even to pain or other stimulation — while 15 is normal.

Coma and brain death are not the same, but people who have coma may progress to legal brain death. Legally brain dead individuals also have a GCS of three. People with coma need to have an artificial airway placed as they are unable to protect their own airway. Once that airway is in place, commonly known as a breathing tube or an endotracheal tube (it goes in your trachea or windpipe), people are also attached to a ventilator that does the breathing for them and supplies additional oxygen as needed. Generally, being comatose is a bad prognostic sign and correlates with reduced chances of full neurologic recovery, let alone survival, when it is due to brain injury and not intoxicants from a really wild Saturday night.
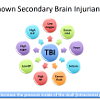
What happens to the cells of your brain after sustaining an impact that creates a brain injury? Kinetic energy is transmitted across your skull to your brain, causing three different conditions for your previously normal brain cells. Some cells are uninjured, and some cells are frankly dead. Nothing may be done for the latter and nothing needs to be done right away for the former. It is the rest of the injured but not dead brain cells that are of concern. How those cells are cared for can strongly influence whether they go on to recover, or progress to being dead. Part of that care involves avoiding things that create more injury; those things are called secondary brain injuriants and the common ones are listed in the graphic below. Secondary brain injuriants are conditions that either make the brain work a lot, inappropriately increase blood flow, or excessively reduce blood flow. Worsened brain injury can lead to brain swelling, which will increase the pressure inside of the skull.

Why, then, would it be beneficial to induce a coma if you have a brain injury and are not already comastose (your GCS is more than eight)? Sometimes, brain injury leads to both bleeding in and around the brain as well as swelling of the brain tissue. Bleeding may require surgery to correct, and less frequently there is surgery to address swelling, as well. A major problem for management is that there are only three things inside your skull: brain, blood and cerebrospinal fluid (CSF, the same stuff that bathes your spinal cord and is sampled during a spinal tap). When any of these elements increases in volume, it squashes the others and can lead to decreased blood flowing to the brain, or even having the brain move out of its normal place within the skull. That process of moving out of the normal location is called herniation and is a life-threatening event. We work very hard to prevent that from happening. This is where inducing a coma may be helpful.
Inducing a coma means that we provide powerful sedatives and analgesics that make you comfortable, control pain, and force your brain to rest. The injured brain is unable to match blood flow to the amount of work it needs to do (normally these are coupled and the process is called auto-regulation). A medical coma reduces the amount of work the injured brain can do, and better matches that work that is required to the reduced amount of blood, and therefore oxygen, that is getting to the brain. The medications also help reduce the risk of seizure after injury. The goal is to allow the injured brain cells to recover.
Since inducing coma is needed in patients who are not awake enough to reliably examine, we need another way to understand if what we are doing is working. That indicator is a pressure monitor that records pressure inside the patient's skull (intra-cranial pressure or ICP). Some of those monitors only measure the pressure, while others can also drain CSF. Even more advanced ones can measure the oxygen in your brain tissue. Clearly, a lot of information helps guide care after severe TBI to help aid in brain recovery.
The Brain Trauma Foundation has performed and collected exhaustive research on how to best manage TBI and has published comprehensive guidelines that are used by trauma centers to care for patients with mild to severe and life-threatening TBI. ICP monitoring and coma induction are a small part of those recommendations for optimal care. As people improve, and using the ICP as a guide, the amount of medications used to induce coma are reduced as the ICP comes back into a more normal range. A lot of other data also factors into the decision to lift the induced coma. That may include changes in the brain CT scan, or how much CSF needs to be drained each day, for example.
Severe brain injury care is complex and takes a team to do well, from the bedside nurse, respiratory therapist, intensivist, neurointensivist, and neurosurgeon to the PharmD, physical therapist, registered dietitian, social worker, case manager — well you get the idea. Yes, it is more like a small village, but trauma centers bring all of the resources needed to bear to save lives and help the critically ill and injured recover.
And yes, people do survive and recover from a medically induced coma. Prognostication is hard, so in general we err on the side of providing hope and life — even if for a while it means making you comatose.